Screening
"Screening" in a medical context refers to the process of identifying apparently healthy individuals who may be at increased risk of a particular disease or condition, so that early intervention or further diagnostic testing can be offered.
Key Principles of Effective Screening Programs
For a screening program to be effective and ethical, several criteria are generally considered (often referred to as the Wilson and Jungner criteria):
The condition should be an important health problem:
It should be common or severe enough to warrant screening.
There should be an accepted treatment for patients with recognized disease
Early detection must lead to a beneficial intervention.
Facilities for diagnosis and treatment should be available
The healthcare system must be able to handle the follow-up.
There should be a recognizable latent or early symptomatic stage:
The disease must have a period where it can be detected before severe symptoms appear.
There should be a suitable test or examination
The screening test must be accurate, safe, acceptable to the population, and cost-effective.
Case-finding should be a continuing process and not a "once and for all" project.
There should be an agreed policy on whom to treat as patients.
The test should be acceptable to the population
People should be willing to undergo the test
The natural history of the condition, including development from latent to declared disease, should be adequately understood.
The cost of case-finding (including diagnosis and treatment of patients identified) should be economically balanced in relation to possible expenditure on medical care as a whole.
Types of Screening:
Population-Based Screening (Mass Screening):
- Applied to a large, unselected population (e.g., all individuals in a certain age group or demographic).
- Examples:
- Cervical Cancer Screening (Pap Smear/HPV Test): For women to detect precancerous changes.
- Breast Cancer Screening (Mammography): For women over a certain age.
- Colorectal Cancer Screening (Fecal Occult Blood Test, Colonoscopy): For adults over a certain age.
- Newborn Screening: For inherited metabolic disorders (e.g., PKU, congenital hypothyroidism) in all newborns.
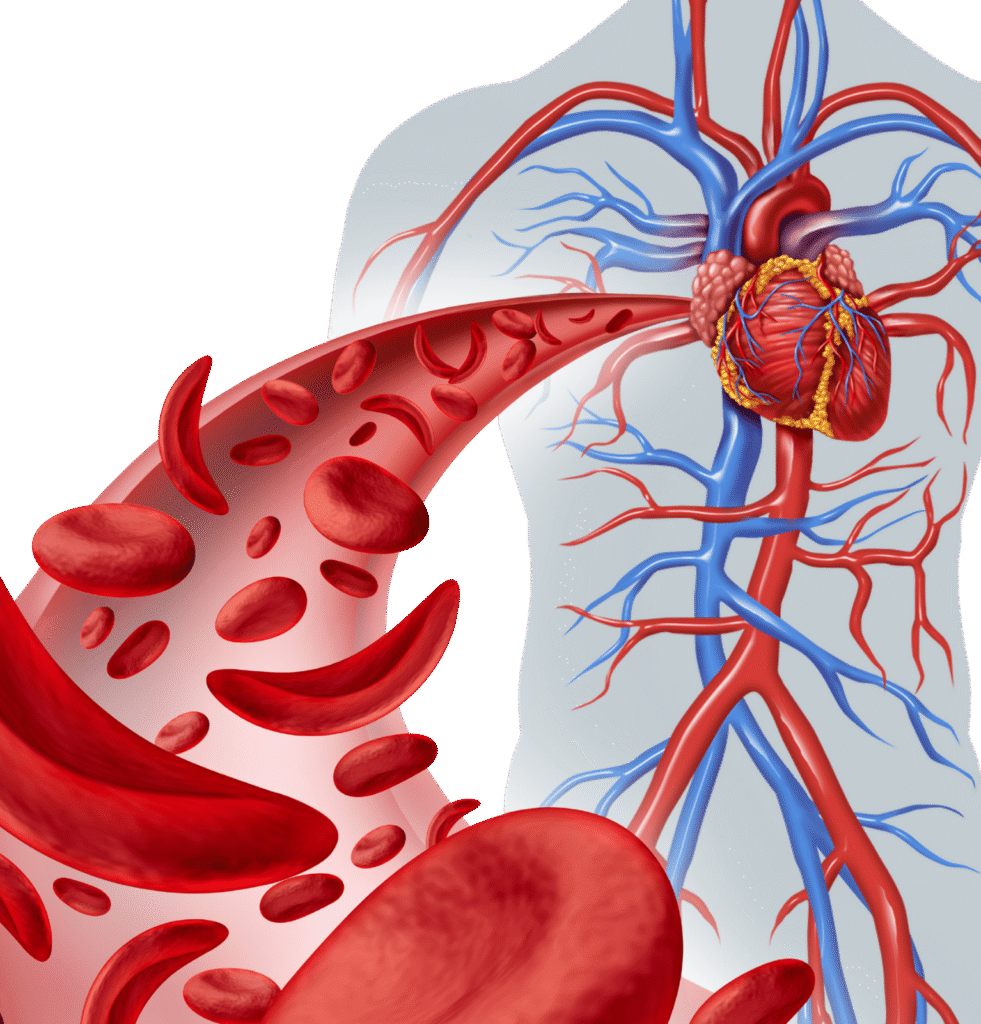
- Blood Pressure Screening: Routine checks for hypertension.
- Cholesterol Screening: For cardiovascular risk.
- Diabetes Screening (Fasting Glucose, HbA1c): For high-risk individuals or general population.
Targeted or Selective Screening:
- Applied to specific subgroups of the population who are at higher risk due to factors like family history, genetics, lifestyle, or environmental exposures.
- Examples:
- Genetic Carrier Screening: For individuals with a family history of a genetic disorder (e.g., Cystic Fibrosis, Sickle Cell Trait) or certain ethnic backgrounds.
- HIV Screening: For individuals with risk factors (e.g., certain sexual behaviors, IV drug use).
- Hepatitis C Screening: For individuals born between certain years or with specific risk factors.
- Osteoporosis Screening (Bone Density Scan): For post-menopausal women or those with risk factors for bone loss.
Role of the Diagnostic Laboratory in Screening
Diagnostic laboratories play a central role in almost all screening programs by:

Performing the Screening Tests
This includes blood tests (e.g., glucose, cholesterol, HbA1c, PSA, specific IgE), urine tests (e.g., urinalysis, microalbumin), molecular tests (e.g., HPV DNA, genetic carrier screening panels), and cytological tests (e.g., Pap smears).
Ensuring Accuracy and Reliability
Providing high-quality, precise, and reliable results is paramount to avoid false positives (leading to unnecessary anxiety and follow-up) and false negatives (missing early disease).
Providing Timely Results
Prompt reporting is essential for early intervention.
Quality Control
Implementing rigorous internal and external quality control measures to maintain test integrity.
Research and Development:
Contributing to the development and validation of new and improved screening methodologies.

