Organ Function Assessment
Organ Function Assessment" refers to the comprehensive evaluation of how well specific organs or organ systems in the body are performing their physiological roles. This is a fundamental aspect of diagnostic medicine, as it helps clinicians:
Diagnose diseases
Identify when an organ is diseased or damaged.
Monitor disease progression
Track how a disease is affecting organ function over time.
Assess treatment effectiveness
Determine if therapies are improving or maintaining organ function.
Screen for conditions
Identify early signs of organ dysfunction before symptoms appear.
Guide medication dosages
Adjust drug levels based on how organs (especially kidneys and liver) metabolize or excrete them.
Evaluate overall health
Provide a general snapshot of a patient's physiological state.
Kidney Function Assessment
The kidneys are vital for filtering waste products from the blood, regulating electrolytes, maintaining fluid balance, and producing hormones.
Key Laboratory Tests:
The bone marrow doesn't produce enough healthy blood cells.
Creatinine (Serum)
A waste product from muscle metabolism; elevated levels indicate reduced kidney filtration.
Blood Urea Nitrogen (BUN)
Another waste product; elevated levels suggest impaired kidney function, dehydration, or other issues.
Estimated Glomerular Filtration Rate (eGFR)
Calculated from serum creatinine (and sometimes age, sex, race), it's the best overall measure of kidney function (how well the kidneys are filtering blood).
Clinical Relevance
Diagnosing Acute Kidney Injury (AKI), Chronic Kidney Disease (CKD), monitoring progression, guiding drug dosing.
Urine Albumin-to-Creatinine Ratio (UACR) / Microalbuminuria
Detects small amounts of protein (albumin) in the urine, an early sign of kidney damage, especially in diabetes and hypertension.
Urinalysis
Checks for protein, blood, glucose, and other substances in the urine, as well as microscopic elements (cells, casts, crystals) that can indicate kidney disease or urinary tract issues.
Electrolytes (Sodium, Potassium, Chloride, Bicarbonate)
Kidneys regulate these; imbalances can indicate kidney dysfunction.
Liver Function Assessment
The liver performs numerous vital functions, including metabolism, detoxification, protein synthesis, and bile production.
Key Laboratory Tests (often called "Liver Function Tests" or LFTs
Alanine Aminotransferase (ALT) and Aspartate Aminotransferase (AST)
Enzymes released when liver cells are damaged. High levels indicate hepatocellular injury.
Alkaline Phosphatase (ALP) and Gamma-Glutamyl Transferase (GGT)
Enzymes often elevated in bile duct obstruction (cholestasis) or liver disease.
Bilirubin (Total and Direct)
A byproduct of red blood cell breakdown; elevated levels cause jaundice and indicate impaired liver processing or bile flow obstruction.
Albumin
A protein synthesized by the liver; low levels can indicate chronic liver disease or malnutrition.
Prothrombin Time (PT) / INR
Measures the time it takes for blood to clot; prolonged time indicates impaired liver synthesis of clotting factors.
Clinical Relevance
Diagnosing hepatitis, cirrhosis, liver failure, bile duct obstruction, monitoring drug toxicity.
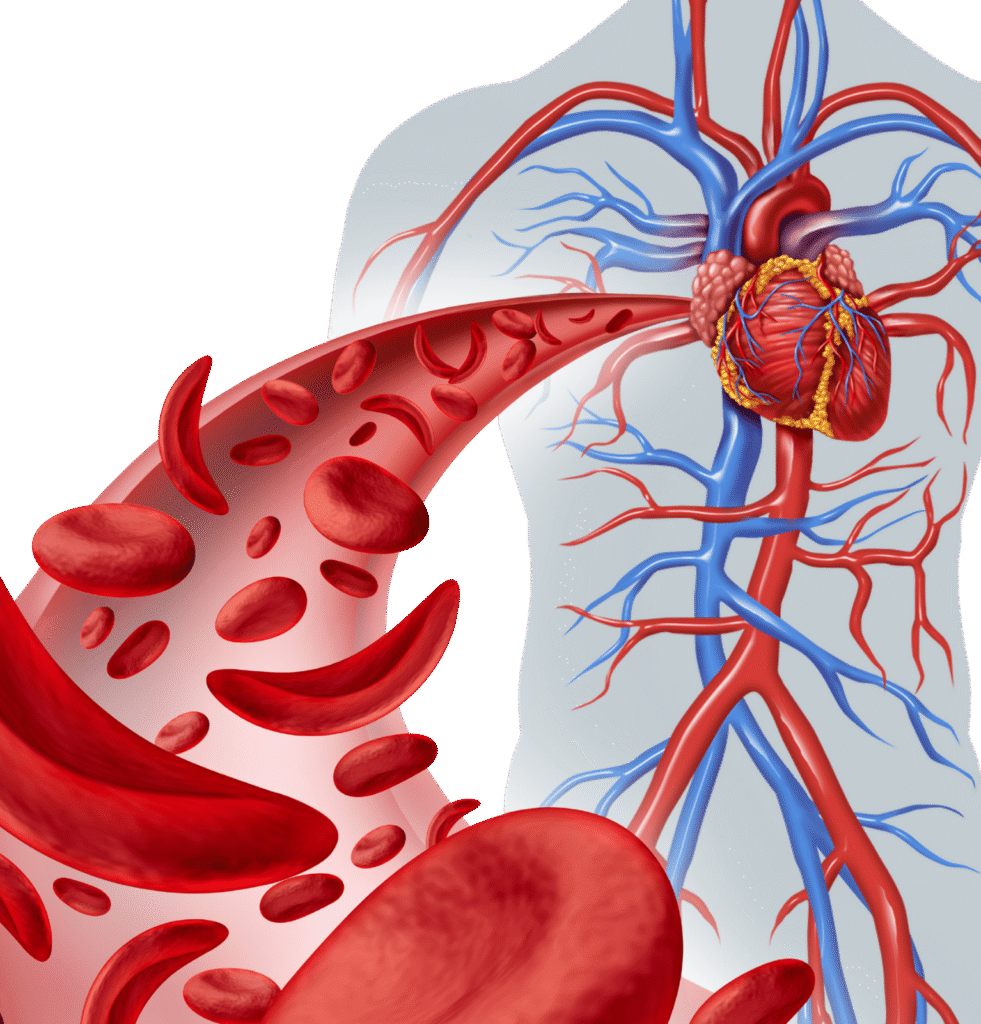
Heart Function Assessment
The heart's primary role is to pump blood throughout the body.
Key Laboratory Tests
Troponin (Cardiac Troponin I or T)
Specific biomarkers released into the blood when heart muscle is damaged (e.g., during a heart attack).
B-type Natriuretic Peptide (BNP) / N-terminal pro-BNP (NT-proBNP):
Hormones released by the heart in response to stretching and stress; elevated levels indicate heart failure.
Lipid Panel (Cholesterol, Triglycerides, HDL, LDL
Assesses cardiovascular risk factors.
C-Reactive Protein (CRP) / High-Sensitivity CRP (hs-CRP):
Non-specific inflammatory marker, but hs-CRP can indicate cardiovascular inflammation and risk.
Clinical Relevance
Diagnosing heart attack, heart failure, assessing cardiovascular risk.
Other Assessments
ECG, Echocardiogram, Stress Test, Cardiac MRI.
Pancreatic Function Assessment
The pancreas has two main functions: producing digestive enzymes (exocrine) and hormones like insulin (endocrine).
Key Laboratory Tests

Amylase and Lipase
Enzymes released into the blood when the pancreas is inflamed or damaged (e.g., in pancreatitis). Lipase is generally more specific for pancreatic issues.
Glucose (Fasting, Random, Oral Glucose Tolerance Test - OGTT, HbA1c
Assesses the endocrine function (insulin production) of the pancreas, crucial for diagnosing diabetes.
Fecal Elastase
Measures pancreatic enzyme activity in stool, indicating exocrine pancreatic insufficiency.
Thyroid Function Assessment
The thyroid gland produces hormones (T3 and T4) that regulate metabolism.
Key Laboratory Tests

Thyroid Stimulating Hormone (TSH)
The most sensitive screening test. High TSH indicates an underactive thyroid (hypothyroidism); low TSH indicates an overactive thyroid (hyperthyroidism).
Free T4 (Thyroxine) and Free T3 (Triiodothyronine)
Measure the active, unbound forms of thyroid hormones. Used to confirm thyroid dysfunction and differentiate types.
Thyroid Antibodies (e.g., Anti-TPO, Anti-Thyroglobulin, TRAb)
Diagnosing hypothyroidism, hyperthyroidism, autoimmune thyroid diseases.
Clinical Relevance
Diagnosing pancreatitis, pancreatic insufficiency, diabetes.
Adrenal Function Assessment
The adrenal glands produce hormones like cortisol, aldosterone, and androgens.
Key Laboratory Tests

Cortisol (Serum, Urine, Saliva)
Measured at specific times (e.g., morning, evening, 24-hour urine) or after stimulation/suppression tests to assess adrenal cortex function (e.g., for Cushing's syndrome or Addison's disease).
ACTH (Adreno corticotropic Hormone
A pituitary hormone that stimulates cortisol production; helps differentiate primary from secondary adrenal disorders.
Aldosterone and Renin
Measured to assess the renin-angiotensin-aldosterone system, important for blood pressure regulation.
Clinical Relevance
Diagnosing adrenal insufficiency, Cushing's syndrome, Conn's syndrome.

