Key Immunohematology Tests
Here are some of the most common and important immunohematology tests, along with their purpose:
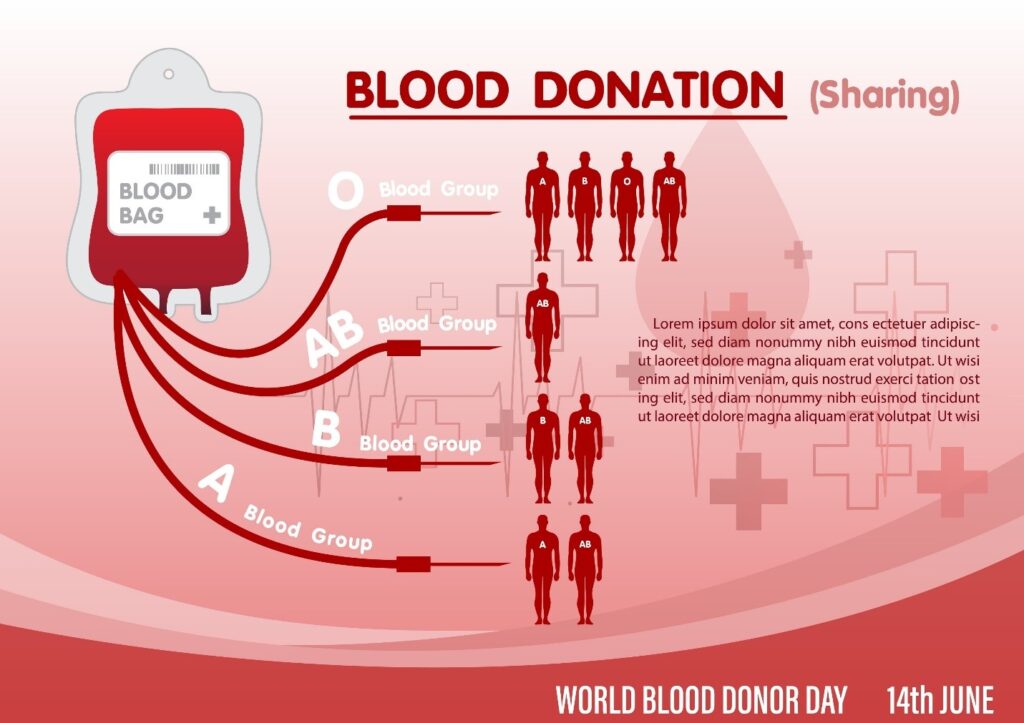
ABO Blood Typing
This is the most fundamental test in blood banking. It determines an individual's blood type (A, B, AB, or O) and whether their blood is Rh-positive or Rh-negative. This is done by testing a blood sample with antibodies against A and B antigens. The clumping (agglutination) or lack thereof indicates the blood type. This test is essential for ensuring a safe blood transfusion, as transfusing an incompatible blood type can be life-threatening.
Antibody Screen (Indirect Antiglobulin Test or IAT)
This test is used to check for the presence of unexpected antibodies in a person's plasma. These antibodies can be formed after a previous transfusion, pregnancy, or in some cases, due to certain diseases. The test involves mixing the patient's plasma with reagent red blood cells that have known antigens. If the patient's plasma contains antibodies, they will bind to the antigens on the reagent cells, and a reaction will be observed. The purpose of this test is to identify these antibodies to prevent a transfusion reaction.
Direct Antiglobulin Test (DAT)
Unlike the antibody screen, which looks for antibodies floating in the plasma, the DAT checks for antibodies already attached to a person's red blood cells. It's often used to investigate conditions like autoimmune hemolytic anemia, hemolytic disease of the fetus and newborn (HDFN), or a transfusion reaction. The test involves taking a sample of the patient's red blood cells and adding a special reagent (Coombs reagent). If the red blood cells are coated with antibodies, they will clump together.
Crossmatch
A crossmatch is the final compatibility check performed before a blood transfusion. The major crossmatch involves mixing a sample of the recipient's plasma with a sample of the donor's red blood cells. The mixture is observed for any sign of clumping or hemolysis (destruction of red blood cells), which would indicate an incompatible reaction. The purpose is to ensure the specific unit of blood being given to the patient is safe and won't cause an immediate or delayed reaction. A minor crossmatch, while not as critical as a major crossmatch, may be done in some circumstances.