Disease Diagnosis
"Disease diagnosis" is the process of identifying the nature and cause of a disease or condition. It involves a systematic approach where healthcare professionals gather information, analyze data, and use their knowledge and experience to determine what is wrong with a patient.
Key Components of Disease Diagnosis:
It's essentially the detective work of medicine, aiming to pinpoint the specific illness responsible for a patient's symptoms.
Patient History (Anamnesis)
- Chief Complaint: The primary reason the patient is seeking medical attention.
- History of Present Illness (HPI): Detailed chronological account of the symptoms, their onset, duration, severity, aggravating/alleviating factors, and associated symptoms.
- Past Medical History (PMH): Previous illnesses, surgeries, hospitalizations, chronic conditions.
- Medications: Current and past medications (prescription, over-the-counter, supplements).
- Allergies: Known allergies to medications, foods, or environmental factors.
- Family History: Medical conditions in close relatives (genetic predispositions).
- Social History: Lifestyle factors (smoking, alcohol, drug use, diet, exercise), occupation, travel history, living conditions, social support.
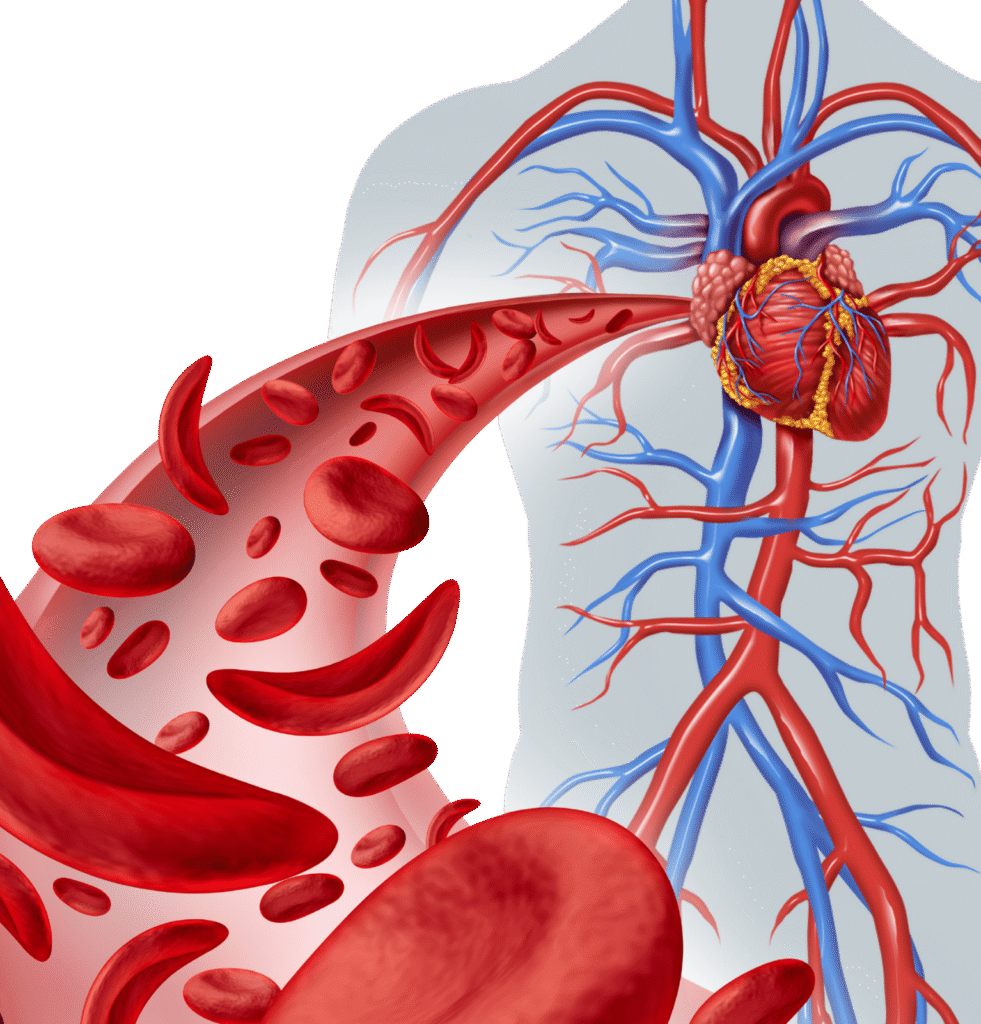
- Review of Systems (ROS): A systematic inquiry about symptoms in different body systems (e.g., cardiovascular, respiratory, gastrointestinal, neurological).
Physical Examination:
- A systematic assessment of the patient’s body using observation, palpation (touch), percussion (tapping), and auscultation (listening).
- Vital Signs: Temperature, blood pressure, heart rate, respiratory rate.
- General Appearance: Overall impression of the patient’s health.
- System-Specific Exams: Detailed examination of relevant body systems based on symptoms (e.g., cardiac exam, lung exam, abdominal exam, neurological exam).
Differential Diagnosis
- Based on the initial information (history and physical), the clinician develops a list of possible diseases that could explain the patient’s symptoms.
- Diagnostic tests are then ordered strategically to narrow down this list and arrive at the most likely diagnosis.
Clinical Reasoning and Judgement
- The clinician integrates all the information from history, physical exam, and diagnostic tests.
- They use their medical knowledge, experience, and critical thinking skills to interpret the findings and formulate a diagnosis.
- Sometimes, a definitive diagnosis may require observation over time or a response to empirical treatment.
Diagnostic Tests
- These are objective tools used to confirm or rule out a suspected diagnosis, assess organ function, identify pathogens, or detect biomarkers.
- Laboratory Tests (Blood, Urine, Other Fluids):
- Hematology: CBC, blood smear, coagulation tests.
- Clinical Chemistry: Electrolytes, glucose, kidney function (creatinine, BUN), liver function (ALT, AST), lipid panel.
- Immunology/Serology: Antibody tests for infections (e.g., HIV, Hepatitis), autoantibodies for autoimmune diseases (e.g., ANA, RF).
- Microbiology: Cultures (blood, urine, sputum), Gram stains, molecular tests (PCR for bacteria, viruses).
- Molecular Biology/Genetics: Gene sequencing, FISH, PCR for genetic disorders or cancer mutations.
- Urinalysis: Physical, chemical, and microscopic examination of urine.
- Histopathology/Cytopathology: Microscopic examination of tissue biopsies or cells (e.g., Pap smear, FNA).
- Imaging Studies:
- X-rays: For bones, lungs.
- Ultrasound: For soft tissues, organs (e.g., abdomen, heart, blood vessels).
- CT Scans (Computed Tomography): Detailed cross-sectional images.
- MRI (Magnetic Resonance Imaging): Detailed images of soft tissues, brain, spinal cord, joints.
- PET Scans (Positron Emission Tomography): Detects metabolic activity, often used in cancer.
- Other Diagnostic Procedures:
- ECG/EKG: For heart electrical activity.
- Endoscopy: Visualizing internal organs (e.g., colonoscopy, gastroscopy).
- Biopsies: Taking tissue samples for microscopic examination.
Importance of Accurate Disease Diagnosis:

Effective Treatment
A correct diagnosis is the prerequisite for effective and targeted treatment. Without it, treatment might be ineffective, harmful, or delayed.
Patient Safety
Prevents unnecessary procedures, inappropriate medications, and potential harm from misdiagnosis.
Prognosis and Counseling:
Provides information about the likely course of the disease and allows for appropriate patient and family counseling.
Public Health
Accurate diagnosis of infectious diseases is crucial for tracking outbreaks, implementing control measures, and preventing spread.
Resource Allocation
Guides the efficient use of healthcare resources.

