Diagnosis of Parasitic Infections
"Diagnosis of Parasitic Infections" involves identifying the presence of parasitic organisms in a host (human or animal) to confirm an infection. Parasites are diverse organisms, ranging from microscopic single-celled protozoa to macroscopic multicellular worms (helminths) and ectoparasites. The diagnostic approach varies significantly depending on the suspected parasite and the affected body system.
Key Principles of Diagnosis
Blood safety involves a multi-layered approach, often described as a "vein-to-vein" or "donor-to-recipient" process:
Key Principles of Diagnosis
Clinical Suspicion
Based on patient symptoms, travel history, dietary habits, exposure to vectors (e.g., mosquitoes, ticks), and epidemiological context.
Specimen Collection
Obtaining the appropriate sample from the site where the parasite or its products are likely to be found.
Laboratory Methods
Employing various techniques to detect the parasite itself, its components (antigens, DNA), or the host's immune response (antibodies).
Common Methods for Diagnosing Parasitic Infections:
Blood safety involves a multi-layered approach, often described as a "vein-to-vein" or "donor-to-recipient" process:
Direct Detection of the Parasite (or its life stages):
This is often the gold standard as it directly confirms the presence of the pathogen.
- Microscopic Examination:
- Stool Examination for Ova and Parasites (O&P):
- Purpose: The most common method for diagnosing intestinal parasitic infections (e.g., Giardiasis, Amoebiasis, Cryptosporidiosis, Hookworm, Ascaris, Tapeworms).
- Method: Microscopic examination of fresh or preserved stool samples to identify parasite eggs (ova), larvae, cysts, or trophozoites. Concentration techniques are often used to increase sensitivity.
- Clinical Importance: Essential for diagnosing a wide range of intestinal parasites.
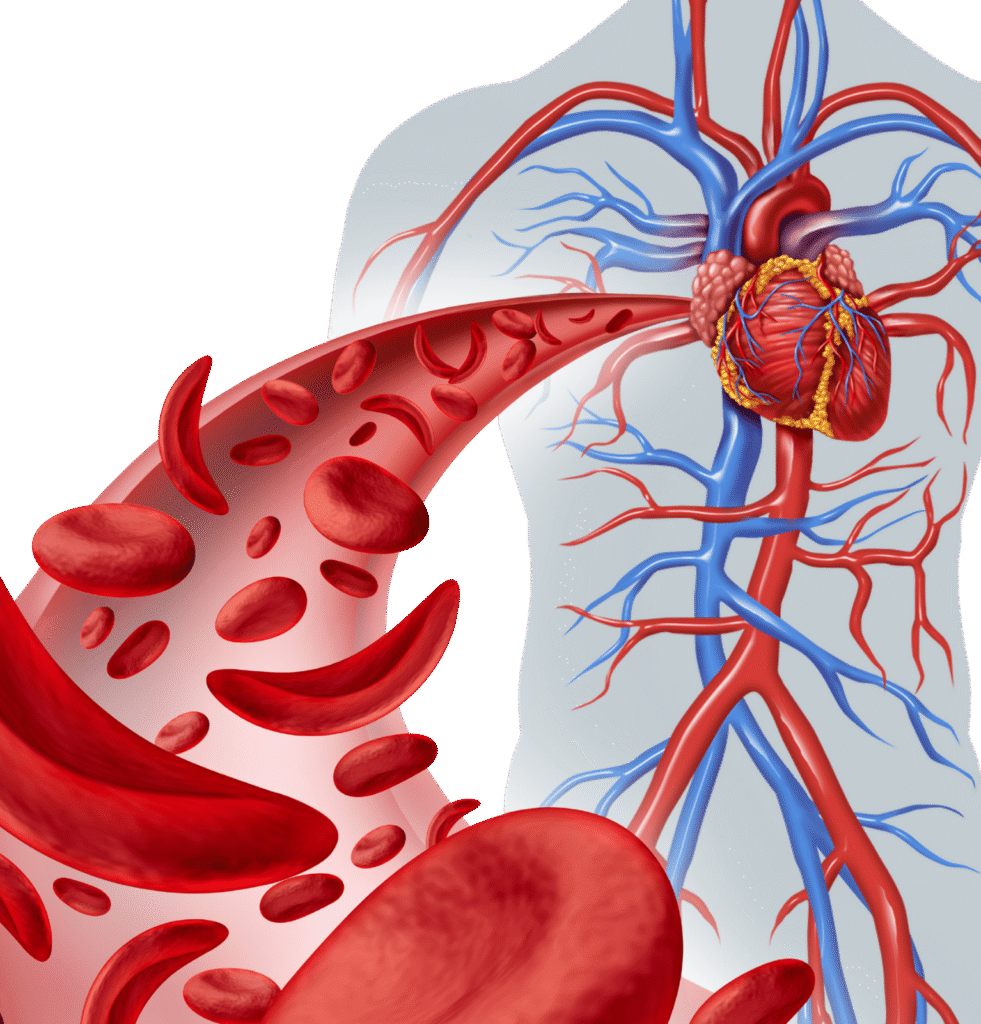
- Blood Smear Examination:
- Purpose: Diagnosing blood parasites (e.g., Malaria, Trypanosomiasis, Filariasis).
- Method: Thick and thin blood smears are stained (e.g., Giemsa stain) and examined under a microscope. Thick smears are for detecting presence, thin smears for species identification and quantification.
- Clinical Importance: Gold standard for malaria diagnosis; crucial for other systemic parasitic infections.
- Other Body Fluids/Tissues:
- Cerebrospinal Fluid (CSF): For parasites causing CNS infections (e.g., Naegleria fowleri, Trypanosoma brucei).
- Urine: For Schistosoma haematobium
- Sputum: For Paragonimus
- Tissue Biopsy/Aspiration: For parasites in specific organs (e.g., liver biopsy for amoebic abscess, muscle biopsy for trichinellosis, skin biopsy for leishmaniasis).
- Scotch Tape Test: For pinworm (Enterobius vermicularis) eggs collected from the perianal region.
- Clinical Importance: Direct visualization provides definitive proof of infection.
- Stool Examination for Ova and Parasites (O&P):
- Antigen Detection Tests:
- Purpose: Detect specific parasite proteins (antigens) in various samples.
- Methods: Rapid diagnostic tests (RDTs) often using immunochromatographic strips (lateral flow assays) or ELISA.
- Examples:
- Malaria RDTs: Detect Plasmodium antigens in blood.
- Giardia/Cryptosporidium Antigen Tests: Detect antigens in stool.
- Amoebic Antigen Tests: Detect Entamoeba histolytica antigen in stool.
- Clinical Importance: Provide rapid results, useful for point-of-care testing or initial screening, especially in endemic areas.
- Molecular Methods (Nucleic Acid Detection):
- Purpose: Detect the parasite’s genetic material (DNA or RNA). Highly sensitive and specific.
- Methods: Polymerase Chain Reaction (PCR), real-time PCR, nested PCR.
- Examples:
- Malaria PCR: More sensitive than microscopy for low parasitemia, species identification.
- Leishmania PCR: From tissue biopsies or blood.
- Chagas Disease PCR: For Trypanosoma cruzi.
- Giardia/Cryptosporidium PCR: In stool.
- Clinical Importance: Useful for low parasite loads, identifying species/strains, and when microscopy is inconclusive. Increasingly used for definitive diagnosis.
Indirect Detection (Host Immune Response):
These tests detect antibodies produced by the patient's immune system in response to the parasitic infection. They indicate exposure but not necessarily active infection (as antibodies can persist after treatment).
Serology (Antibody Detection)
Purpose
Detects specific IgG or IgM antibodies against a parasite.
Methods
ELISA, Indirect Immunofluorescence Antibody Test (IFA), Western Blot.
Clinical Importance
Useful for systemic or invasive parasitic infections where direct detection is difficult, or for screening populations.
Examples:
- Toxoplasmosis: IgG (past infection/immunity), IgM (recent/acute infection).
- Cysticercosis (Tapeworm larvae): Antibodies in serum or CSF.
- Echinococcosis (Hydatid disease):
- Schistosomiasis:
- Amoebic Liver Abscess: Antibodies (often positive in invasive disease).
Challenges in Diagnosis
Accurate diagnosis of parasitic infections is crucial for initiating appropriate antiparasitic treatment, preventing complications, and implementing public health measures to control spread.

Intermittent Shedding
Some parasites shed eggs or cysts intermittently, requiring multiple stool samples.
Low Parasite Load
In chronic infections or early stages, parasite numbers may be low, making direct detection difficult.
Morphological Similarity
Some parasite species look very similar under the microscope.
Lack of Specific Symptoms
Symptoms can be non-specific, mimicking other conditions.
Geographic Distribution
Awareness of locally endemic parasites is important.
Test Availability
Advanced molecular or serological tests may not be available in all settings.

