Cancer Diagnosis & Monitoring
"Cancer Diagnosis & Monitoring" encompasses the entire journey of identifying cancer, determining its characteristics, tracking its response to treatment, and watching for any signs of recurrence. This process is highly complex and relies heavily on a multidisciplinary approach, with diagnostic laboratories playing a central and indispensable role.
What is Cancer?
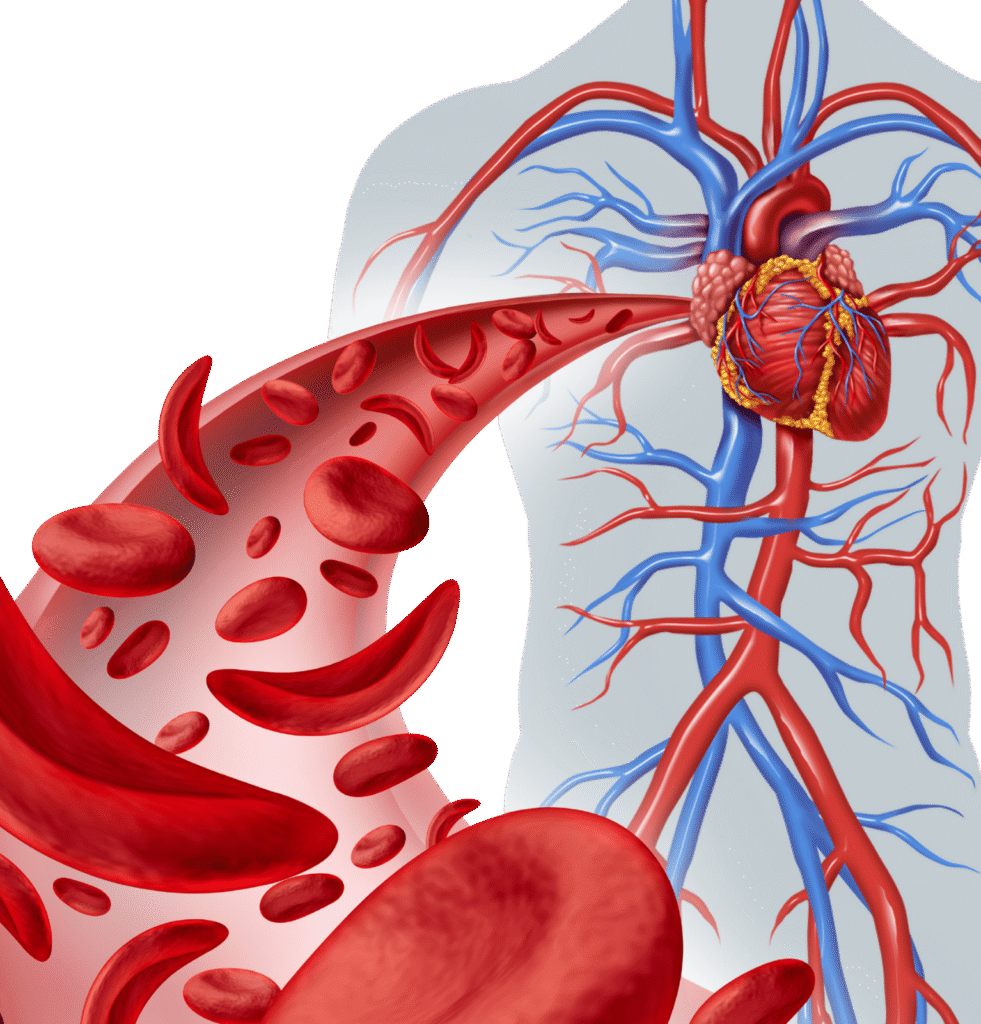
Cancer is a disease characterized by the uncontrolled growth and spread of abnormal cells in the body. These abnormal cells, unlike healthy cells, do not follow normal cell cycle controls, can invade surrounding tissues, and can metastasize (spread) to distant parts of the body through the bloodstream or lymphatic system.
Stem Cell Niche
Provides the environment and support for stem cells to differentiate and mature.
Immune Cell Production
Produces lymphocytes, which are critical components of the immune system.
Cancer Diagnosis
Once cancer is diagnosed and treatment begins, continuous monitoring is essential to track the disease's response to therapy, detect any recurrence, and manage complications.
Initial Suspicion
- Symptoms: Patients may present with various non-specific symptoms (e.g., unexplained weight loss, fatigue, persistent pain, new lumps, changes in bowel habits) or more specific symptoms related to the affected organ.
- Screening Programs: Routine screenings (e.g., mammography for breast cancer, Pap test for cervical cancer, colonoscopy for colorectal cancer, PSA for prostate cancer) aim to detect cancer early, often before symptoms appear.
Molecular Diagnostics in Cancer Diagnosis
- Purpose: To identify specific genetic mutations, chromosomal rearrangements, or gene amplifications within cancer cells. This information is crucial for:
- Sub-classification: More precise classification of cancer types (e.g., specific subtypes of lung cancer, leukemia).
- Prognosis: Predicting disease behavior.
- Targeted Therapy: Identifying patients who will respond to specific drugs that target these molecular alterations (e.g., EGFR mutations in lung cancer, HER2 amplification in breast cancer, BRAF mutations in melanoma).
- Methods: Fluorescence In Situ Hybridization (FISH), Polymerase Chain Reaction (PCR), Next-Generation Sequencing (NGS) (e.g., cancer gene panels, whole exome sequencing).
Key Diagnostic Methods
- Biopsy (The Gold Standard):
- What it is: The definitive method for diagnosing most cancers. It involves removing a small sample of suspicious tissue or cells from the body.
- Types: Incisional biopsy, excisional biopsy, core needle biopsy, fine needle aspiration (FNA), endoscopic biopsy, bone marrow biopsy.
- Role of Pathology: The tissue/cell sample is sent to the Histopathology or Cytopathology laboratory for microscopic examination.
- Histopathology: Pathologists examine tissue architecture and cellular morphology to confirm malignancy, determine the specific type of cancer (e.g., adenocarcinoma, squamous cell carcinoma), and assess its grade (how aggressive it looks).
- Cytopathology: Pathologists examine individual cells obtained from fluids, brushings, or FNAs for malignant features.
- Imaging Studies:
- Purpose: To locate tumors, determine their size and extent, assess involvement of surrounding tissues, and detect spread (metastasis).
- Examples: X-rays, Ultrasound, Computed Tomography (CT) scans, Magnetic Resonance Imaging (MRI), Positron Emission Tomography (PET) scans (often combined with CT, PET-CT).
- Laboratory Tests (Blood, Urine, Other Fluids):
- Tumor Markers: Substances (proteins, hormones, enzymes) produced by cancer cells or by the body in response to cancer. While rarely diagnostic on their own, they can raise suspicion and are very useful for monitoring.
- Examples: Prostate-Specific Antigen (PSA) for prostate cancer, Carcinoembryonic Antigen (CEA) for colorectal cancer, CA 125 for ovarian cancer, Alpha-Fetoprotein (AFP) for liver or germ cell tumors, Beta-HCG for germ cell tumors, M-protein/Free Light Chains for Multiple Myeloma.
- Blood Counts (CBC): Can reveal anemia, abnormal white blood cell counts (leukemia, lymphoma), or low platelet counts, which might be signs of bone marrow involvement or blood cancers.
- Organ Function Tests: To assess if cancer is affecting organ function (e.g., kidney function tests if kidney cancer or myeloma is suspected, liver function tests if liver metastases).
- Tumor Markers: Substances (proteins, hormones, enzymes) produced by cancer cells or by the body in response to cancer. While rarely diagnostic on their own, they can raise suspicion and are very useful for monitoring.
Cancer Monitoring
The process of diagnosing cancer typically begins with a suspicion based on symptoms or screening results and progresses through several stages to confirm the presence of cancer, identify its type, and determine its extent.
Clinical Monitoring
- Symptoms: Regular assessment of symptoms, pain levels, and overall well-being.
- Physical Examination: Checking for new lumps, swollen lymph nodes, or other physical signs.
Imaging Monitoring
- Purpose: To assess changes in tumor size, detect new lesions, or evaluate the extent of metastasis.
- Frequency: Varies based on cancer type, stage, and treatment regimen (e.g., CT scans, MRI, PET-CT scans at regular intervals).
Laboratory Monitoring
- Tumor Markers:
- Purpose: The most common lab test for monitoring. A decrease in tumor marker levels often indicates a positive response to treatment, while a rise can signal disease progression or recurrence.
- Examples: PSA, CEA, CA 125, AFP, Beta-HCG, M-protein/Free Light Chains.
- Important Note: Tumor markers are not perfect; they can be elevated in non-cancerous conditions and not all cancers produce them. They are generally used in conjunction with other monitoring methods.
- Complete Blood Count (CBC) and Blood Chemistry:
- Purpose: To monitor for side effects of chemotherapy or radiation (e.g., myelosuppression leading to low blood counts), assess organ function (kidney, liver) that might be affected by cancer or treatment, and detect complications like hypercalcemia.
- Liquid Biopsy (Circulating Tumor DNA – ctDNA):
- Purpose: A non-invasive blood test that detects fragments of tumor DNA released into the bloodstream by cancer cells.
- Clinical Importance: Increasingly used for:
- Monitoring Treatment Response: Changes in ctDNA levels can reflect tumor burden.
- Detecting Minimal Residual Disease (MRD): Identifying very small amounts of cancer cells remaining after treatment, even when other tests show remission.
- Detecting Early Relapse: ctDNA levels may rise before imaging or tumor markers show recurrence.
- Identifying Resistance Mutations: Detecting new mutations that emerge during treatment, which might explain treatment failure and guide a change in therapy.
- Minimal Residual Disease (MRD) Testing:
- Purpose: Highly sensitive tests (often molecular or flow cytometry) to detect tiny numbers of cancer cells that remain after treatment, particularly in blood cancers like leukemia and lymphoma.
Clinical Importance: MRD negativity is often associated with better outcomes and can guide decisions about further treatment or surveillance.

