Bleeding Disorders
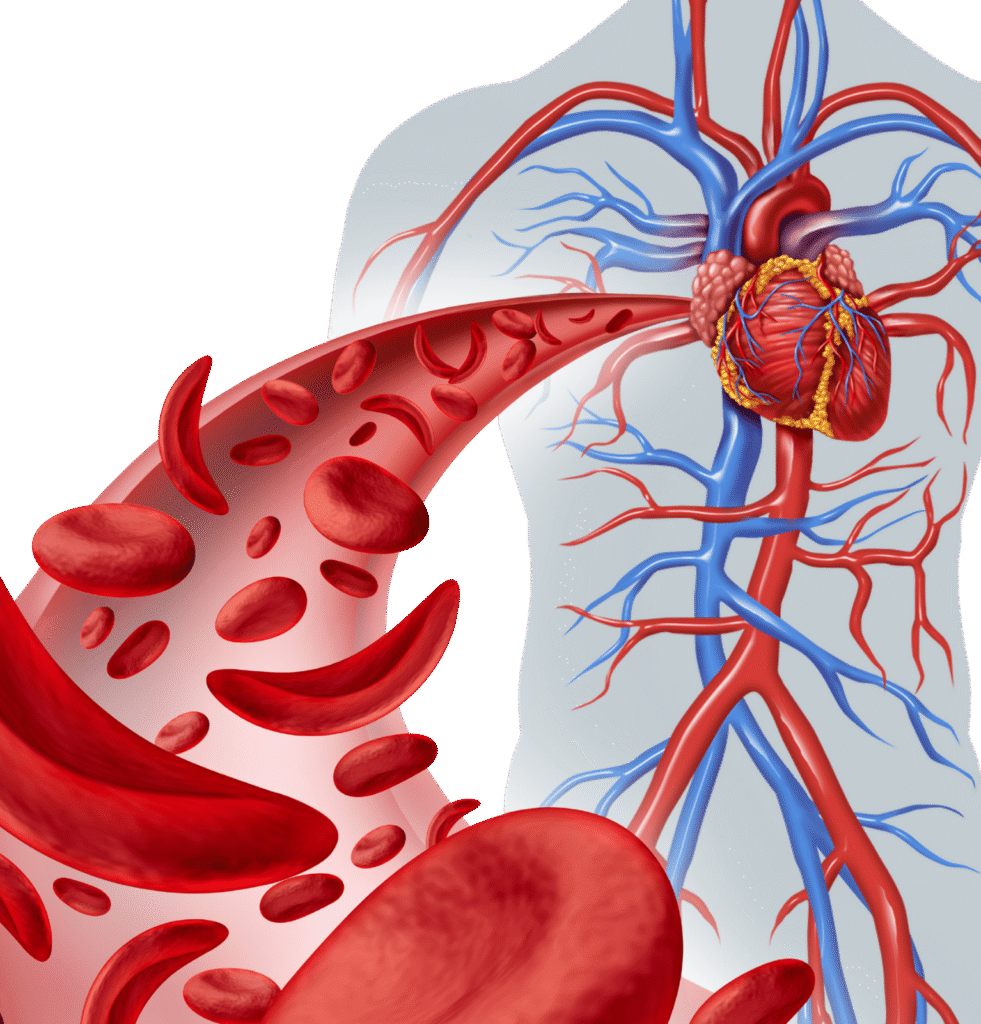
"Bleeding disorders" are a group of conditions where the body's natural process of blood clotting (hemostasis) is impaired, leading to prolonged or excessive bleeding. This impairment can result from deficiencies or defects in blood vessels, platelets, or coagulation factors.
The Normal Clotting Process (Hemostasis) involves three main steps:
Vascular Spasm
Blood vessels constrict to reduce blood flow to the injured area.
Platelet Plug Formation
Platelets (small cell fragments in the blood) adhere to the injured vessel wall and to each other, forming a temporary plug.
Coagulation (Clot Formation):
A complex cascade of proteins called coagulation factors (or clotting factors) interact to form a stable fibrin clot, which reinforces the platelet plug and stops the bleeding.
Types of Bleeding Disorders
Bleeding disorders can be broadly categorized based on the component of the clotting system that is affected:
Platelet Disorders
These involve problems with the number or function of platelets.
Thrombocytopenia
Cause
Low platelet count. This can be due to decreased production in the bone marrow (e.g., aplastic anemia, leukemia, chemotherapy, viral infections like dengue), increased destruction (e.g., Immune Thrombocytopenic Purpura (ITP), drug-induced thrombocytopenia), or sequestration (e.g., in an enlarged spleen).
Symptoms
Petechiae (tiny red spots), purpura (larger bruises), mucosal bleeding (nosebleeds, gum bleeding), prolonged bleeding from minor cuts.
Platelet Function Disorders (Thrombocytopathy)
Cause
Normal platelet count, but the platelets don't function properly (e.g., they don't stick together or to the vessel wall effectively). Can be inherited (e.g., Glanzmann's thrombasthenia, Bernard-Soulier syndrome) or acquired (e.g., due to medications like aspirin, NSAIDs, or kidney disease).
Symptoms
Similar to thrombocytopenia, but bleeding time is prolonged.
Coagulation Factor Disorders
These involve deficiencies or defects in the proteins (coagulation factors) necessary for forming a stable fibrin clot.
Hemophilia (e.g., Hemophilia A, Hemophilia B)
Cause
The most well-known inherited bleeding disorder.
Hemophilia A: Deficiency of Factor VIII (most common type).
Hemophilia B: Deficiency of Factor IX.
Symptoms
Spontaneous bleeding into joints (hemarthrosis), muscles, and soft tissues; prolonged bleeding after injury or surgery; internal bleeding. Severity varies.
Von Willebrand Disease (VWD
Cause
The most common inherited bleeding disorder. Deficiency or defect in von Willebrand factor (vWF), a protein that helps platelets stick to the vessel wall and also carries Factor VIII.
Symptoms
Often milder than hemophilia, including easy bruising, nosebleeds, heavy menstrual bleeding, prolonged bleeding after surgery/dental work.
Rare Factor Deficiencies
Deficiencies in other clotting factors
(e.g., Factor I/fibrinogen, Factor II/prothrombin, Factor VII, Factor X, Factor XI, Factor XIII). These are less common but can cause significant bleeding.
Acquired Coagulation Factor Deficiencies:
Liver Disease
The liver produces most clotting factors, so severe liver disease can lead to multiple factor deficiencies.
Vitamin K Deficiency
Vitamin K is essential for the production of Factors II, VII, IX, and X. Deficiency can be due to poor diet, malabsorption, or certain medications (e.g., warfarin overdose).
Vascular Disorders
A complex, life-threatening condition where widespread activation of the clotting system leads to consumption of clotting factors and platelets, resulting in both bleeding and clotting simultaneously. Triggered by severe underlying conditions like sepsis, trauma, or cancer.
Vascular Disorders
These involve abnormalities in the blood vessels themselves.

Hereditary Hemorrhagic Telangiectasia (HHT):
Cause
Inherited disorder causing fragile, dilated blood vessels (telangiectasias) that bleed easily.
Vasculitis
Inflammation of blood vessels, which can lead to bleeding.
Scurvy
Vitamin C deficiency, leading to fragile capillaries.
Diagnosis of Bleeding Disorders
Patient history
Detailed questions about bleeding episodes, family history.
Physical examination
Varies, often normocytic. Positive Direct Antiglobulin Test (DAT/Coombs test).
Laboratory tests
Complete Blood Count (CBC):
To check platelet count.
Prothrombin Time (PT) and International Normalized Ratio (INR)
Assess extrinsic and common coagulation pathways.
Activated Partial Thromboplastin Time (aPTT):
Assess intrinsic and common coagulation pathways.
Bleeding Time or Platelet Function Analyzer (PFA-100)
Assess platelet function.
Specific Factor Assays
To measure levels of individual clotting factors.
Von Willebrand Factor Assays
To diagnose VWD.
Platelet Aggregation Studies
To assess platelet function.

